Diabetic neuropathy and polyneuropathy
Scientific support: Dr. Gidon Bönhof
Diabetic neuropathy encompasses various pathologies in which nerves in various parts of the body are damaged by elevated blood sugar levels. As a result, certain bodily functions controlled by nerves no longer work. If several nerves are affected, medical professionals refer to this as polyneuropathy.
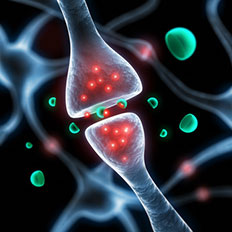
Like electrical cables, nerves connect our brain with muscles, sensors in the skin, and other organs. Through the nerves, the brain transmits control signals to even the smallest parts of the body. Our skin contains small sensors that transmit sensations to the brain via nerve pathways.
The nerve disorders associated with diabetes can affect many parts of the nervous system. Correspondingly, this can be characterized by different clinical pictures. There are two main categories:
- Diabetic peripheral neuropathy (affecting the nerves responsible for muscle movement and the sensitivity of the skin)
- Diabetic autonomic neuropathy (affecting the nerves that control the organs in the body)
Depending on which area is affected, patients may suffer numbness or pain in their hands and feet. Neuropathic disorders can also affect digestion or the heartbeat. It is common for such disorders to remain undiscovered during the early stages.
For patients with type 1 diabetes, good blood sugar management and a healthy lifestyle can help prevent the onset of neuropathic disorders. A medical examination is required when the first symptoms appear. Neuropathic disorders cannot be directly prevented in patients with type 2 diabetes. Various treatment options can be discussed depending on the clinical picture.
The part of the nervous system responsible for movement is known as the voluntary or somatic nervous system. When this part of the nervous system is damaged by diabetes mellitus, this is known as diabetic peripheral neuropathy. Diabetic peripheral neuropathy commonly affects the right and left side of the body to an equal extent.
Those affected often don’t notice any symptoms during the early stages. It is common for peripheral neuropathy to be diagnosed after symptoms have become apparent. The symptoms normally begin in the feet and lower legs and less commonly in the hands and arms.
Good to know:
Most of the symptoms can also be found in other diseases. A medical examination can exclude any other pathologies.
Diabetic peripheral neuropathy can manifest itself in a variety of ways. In some people, their perception of touch, temperature differences and pain stimuli is impaired. Because the nerves transmit fewer signals to the brain, these are known as negative symptoms. Around the half of all those affected develop sensory disturbances, such as tingling, numbness, or even severe pain. These sensory disturbances are counted as positive symptoms because additional, but incorrect, sensations are being perceived. The perception of these uncomfortable sensations can be more pronounced when resting, especially in the evening or at night, and less pronounced when moving. Other possible symptoms include weakness in the leg muscles and an uncertain gait. However, there are a wide range of other diseases that produce similar symptoms. This is why a thorough medical examination is essential.
Severe, poorly healing wounds on the feet are common due to the fact that the polyneuropathy makes it more difficult to perceive lesions and pressure sores on the feet. This is known as diabetic foot syndrome.
The part of the nervous system responsible for controlling the function of the internal organs, without our conscious participation, is known as the involuntary or autonomic nervous system. When this part of the nervous system is damaged by diabetes, this is known as diabetic autonomic neuropathy.
The symptoms can vary greatly depending on which organ is affected by the neuropathic disorder. Severe symptoms related to these diseases are less common and tend to appear after suffering diabetes for long period of time.
The cardiovascular system can also be affected by this type of nerve damage. It is common for the heart to beat faster than normal, even when resting. This means that the heart and circulatory system cannot adapt as well to alternating types of exertion, such as strenuous physical activity, and severe stress. Cardiac arrhythmia is also more common, and the risk of stroke and sudden cardiac death is increased. Therefore, it is advisable to avoid medications that reduce the ability of the heart rate to adjust (heart rate variability). Because the symptoms of heart rate variability are very non-specific, cardiovascular function should be subject to an in-depth examination to exclude the presence of other pathologies.
Find out more about cardiovascular disease here!
If there is nerve damage in the gastrointestinal tract, this can result in nausea, a sensation of fullness, or constipation. A common reason for these symptoms is that the nerve damage causes the stomach to empty either too quickly or too slowly. The esophagus, stomach, and intestines transport food using targeted alternating muscle tension and relaxation. All these processes are co-controlled by the nervous system and can therefore be affected by diabetes.
Autonomic neuropathic disorders can also cause problems with emptying the bladder or sexual disorders. Some patients no longer notice when their bladder is full or are unable to fully empty their bladder. Others always feel as though they have to go to bathroom, even though their bladder is not full. Many men and women suffer from sexual dysfunction disorders as a consequence of diabetes.
Find out more about sexual dysfunction disorders here!
Due to the fact that almost all organs in the body are influenced by the nervous system, many more bodily functions can be negatively affected by autonomic nerve damage, including the hormonal system, sweat glands, or eye movement control.
There are a number of factors that can increase the risk for diabetic nerve damage:
- Older age
- Suffering from diabetes over a long period of time
- Long-term elevated blood sugar levels
- Frequent metabolic imbalances during childhood and adolescence
- Vascular diseases
- Eye and kidney diseases associated with diabetes
- Increased blood lipid levels
- High blood pressure
- Smoking
- Alcohol
- Lack of physical activity
- Being overweight
- Poor diet
There are several things people with type 1 diabetes can do to reduce the risk of neuropathic disorders or delay the progression of existing nerve damage. Although the onset of neuropathy cannot be directly prevented in patients with type 2 diabetes, there are some risk factors that can be positively influenced.
- In cases of type 1 diabetes, excellent metabolism management early on via intensified insulin therapy for the beginning and the maintenance of normal blood sugar levels in the long-term have proven to reduce the risk of nerve damage.
Take note: When type 1 diabetes is first diagnosed, the blood sugar levels cannot be reduced too much too quickly.
- There is evidence that sufficient physical activity is able to relieve not only autonomic nerve damage but also the symptoms of peripheral nerve damage. This applies both to people with type 1 and type 2 diabetes.
- A healthy lifestyle is crucial:
- Don’t smoke
- Try to avoid alcohol as much as possible, since alcohol can also cause neuropathic disorders.
- Eat a balanced diet and maintain an overview of the nutrients contained in your foods and drinks.
- Regular physical activity.
- Try to maintain a healthy weight.
People who have already noticed neuropathic symptoms, should visit a doctor (specialist field: neurology) to provide details (what, when, since when, how, where). If they have had diabetes for more than 5 years, doctors will begin by examining people with type 1 diabetes who are in a poor metabolic state to identify potential neuropathic disorders. For children, the first examinations take place at age 11. These examinations are then repeated on a yearly basis. For people with type 2 diabetes with no signs of neuropathic disorders, the doctor will carry out an examination every year to enable the early detection of nerve damage.
These examinations include the detailed description of symptoms and compilation of a medical history, including details of all medications used and accompanying diseases. It is essential to rule out other pathologies or medications as the potential cause of the nerve damage. Orthopedic problems, e.g., a herniated disc, other neurological problems, certain types of medication, or alcohol can all cause nerve damage. It is not always simple to differentiate these cases from diabetes-related nerve damage. If the patient has pain, then the pain intensity must be documented to allow assessment of the progress and the success of any potential course of treatment.
The doctor will then carefully examine the legs and feet to assess, for example, the mobility of the muscles and joints and to test skin sensitivity. Touch sensitivity can be tested using cotton wool or a firm nylon thread. A pointed object is used to test pain sensitivity. Vibration sensitivity is tested using an oscillating tuning fork. A reflex hammer is tapped on the tendons of the knee and heel to determine if the muscle reflexes can be triggered.
If the diagnosis after these simple methods is uncertain, then further special neurological examination can be ordered. Because nerves work like electrical cables, it is possible to test the speed with which they conduct electrical impulses. This is known as the nerve conduction velocity. The test method is known as electroneurography. In rare cases, medical specialists will collect tiny skin and tissue samples from above the ankle to see if the skin contains less nerve fibers than normal.
Autonomic neuropathy
Examinations for the early detection of autonomic neuropathic disorders have been used only rarely outside the field of scientific research. The speed and variability of the pulse can provide important information. However, this requires long-term monitoring of the heartbeat (long-term ECG). This makes it all the more important for patients to describe all possible signs during their consultation and for other causes to be ruled out. If there is evidence of nerve damage in the gastrointestinal tract, bladder, or sexual organs, the patient will be referred to a specialist for the respective organ system.
In many cases, nerve damage cannot be healed or reversed. However, regular screening and early initiation of therapy for preexisting risk factors can positively influence the onset and progression of the disease.
Treatment can prevent or at least delay the progression of diabetic polyneuropathy and relieve the symptoms.
Excellent blood sugar management can delay or stop progression in patients with type 1 diabetes. As soon as a neuropathic disorder is diagnosed, together with their physician, those affected should determine what therapeutic options can be considered. These can vary from person to person. In every case, is it important to rule out as many alternative causes of nerve damage as possible, such as excessive alcohol consumption or vitamin B12 deficiency. In case with pain, the therapy not only aims to reduce the pain levels but also improve overall quality of life via better sleep and improved mobility.
Drug-based therapy
Certain medication can help to relieve the symptoms associated with sensory disturbances and pain. It is important to note: Normal pain medication used for headaches, joint pain, or stomach pain (aspirin, ibuprofen, etc.) is not suitable. Instead, physicians should prescribe other types of medication that have a direct effect on the nervous system, such as pregabalin or duloxetine.
Until the onset of action, if tolerated, the dosage of these medications should not exceed the stated maximum dosage. In practice, it often happens that the therapy is begun using a low dosage and then the dosage increase is forgotten about, despite no symptom relief having been achieved. Therefore, it is important to test the efficiency of the highest possible dosage before switching to another type of medication.
Regarding side effects, careful consideration is necessary to determine to what extent these are justifiable or not. Depending on the type of neuropathic symptoms and accompanying diseases, several different types of medication can be taken in combination. In severe cases, the use of morphine is medically justifiable.
Alongside these symptomatic therapies, there are also approaches that attempt to influence the underlying mechanisms that cause the nerve damage. In various studies, alpha-lipoic acid, a well-tolerable over-the-counter medication, has been shown to have positive effects on nerve function and the symptoms of diabetic peripheral neuropathy. Some studies even report a very rapid improvement. Other studies report that benefits are more likely in the long term. This means that individual therapeutic success is somewhat more difficult to assess.
It is also suspected that benfotiamine, a synthetic derivative of vitamin B1, can positively affect these mechanisms that are assumed to be involved in onset of diabetic nerve damage. It is already in use in the treatment of diabetic neuropathic disorders. Up until now, there are only a few studies available that substantiate the beneficial effects after several weeks of use. Because alpha-lipoic acid and benfotiamine are both freely available at pharmacies in Germany, the costs for both are not reimbursed by the health insurance providers.
Other treatment approaches
Alongside the regular use of medication, other treatment approaches are available. Some patients find psychotherapy helpful in improving the impaired quality of life associated with sensory disturbances or limited mobility. Electrical stimulation using special medical devices can potentially relieve symptoms. Medical professionals call this type of treatment TENS (transcutaneous electrical nerve stimulation). The local application of capsaicin patches can be used in an attempt to treat difficult-to-treat neuropathic pain. Capsaicin is an active component of chili peppers, and it is responsible for the taste we perceive as being hot. Regular physical therapy and physiotherapy can help muscle weakness, mobility disorders, or paralysis. It is important to maintain a basic level of physical activity as the body can unlearn movement processes resulting in increased muscular atrophy.
People who have impaired touch and pain sensitivity in their feet due to polyneuropathy should regularly check their feet and shoes for pressure sores and chaffing. If necessary, insoles or special shoes and regular podiatric foot care should be considered.
Find out more about the treatment of diabetic foot syndrome here!
People with autonomic neuropathy are treated depending on the organ affected. Adapted physical training that is not too strenuous can help with circulatory problems and dizziness. It should also be checked whether other drugs are negatively influencing the symptoms. For example, this is the case with beta blockers and antidepressants.
Tailored nutritional therapy can help if the emptying of the stomach or the digestive processes in the intestines are no longer working correctly. It can also help to split food into several small meals and reduce the amounts of fat and fibers in the diet. Thoroughly chewing food and keeping the upper body upright after eating is also recommended. In serious cases, the use of medications that promote the motility of the stomach can be considered. People who need to inject insulin at mealtimes must be careful not to develop low blood sugar levels as a result of the slowed digestive process.
Diabetes-induced bladder dysfunction can be helped, for example, using behavioral patterns related to voiding the bladder (e.g., urination at certain times of day, urination twice successively at very short intervals). In certain cases, medications can be used, or a catheter must be inserted.
In cases of sexual dysfunction disorders affecting men or women, the medication being used should also be assessed. The circumstances of the patient should also be taken into consideration. Hormonal disorders should be ruled out. Medications can be used to see if they have a positive effect on the patient's sex life.
Find out more about the treatment of sexual dysfunction disorders here!
Scientists continue to research how exactly nerve damage associated with diabetes develops. Nerve damage does not begin when the first symptoms are noticed but occurs unnoticed during the early stages of diabetes.
Medical specialists suspect that a combination of factors is responsible for diabetic neuropathy and polyneuropathy. High blood sugar levels over a long period of time can damage the blood vessels that supply the nerves with nutrients. High blood sugar levels change certain processes in the body, which increases the accumulation of glucose degradation products and the development of highly reactive (radical) oxygen molecules. It is suspected that both are damaging to the nerves.
Generally, diabetes can be accompanied by underlying inflammatory processes throughout the body. Studies were able to show that these processes correlate to poorer nerve function. Overall, the number of peripheral nerve fibers is reduced, for example, in the skin.
According to studies, half of all people with type 2 diabetes will also suffer from diabetic nerve damage in the course of their lifetime.
Around 30 out of every 100 people with type 1 or type 2 diabetes have diabetic polyneuropathy. Depending on the definition applied, approx. 20 to 30 people out of every 100 people with type 1 diabetes and 12 to 22 people out of every 100 people with type 2 diabetes suffer from autonomic neuropathy affecting the cardiovascular system.
Sources:
Bönhof, G. J. et al.: Emerging Biomarkers, Tools, and Treatments for Diabetic Polyneuropathy. In: Endocr Rev, 2019, 40: 153-192
Bundesärztekammer et al.: Nationale Versorgungsleitlinie Neuropathie bei Diabetes im Erwachsenenalter. Langfassung. 1. Auflage. Version 5. 2011
Bundesärztekammer et al.: Patientenleitlinie zur Nationalen Versorgungsleitlinie Nervenschädigungen bei Diabetes. 1. Auflage. Version 1.0. 2014
Deutsche Diabetes Gesellschaft et al.: S3-Leitlinie Diagnostik, Therapie und Verlaufskontrolle des Diabetes mellitus im Kindes- und Jugendalter. Langfassung. 2015
Ziegler, D. et al.: Diabetische Neuropathie. In: Diabetologie, 2018, 13: S230-S243
Ziegler, D.: Kardiovaskuläre autonome diabetische Neuropathie. In: Diabetologie, 2017, 12: 28-42
As of: 30.03.2021






