Insulin therapy: What types of technical aids are available?
Scientific support: Prof. Dr. Andreas Fritsche, Prof. Dr. Barbara Ludwig, Andreas Vosseler M.A.
Most people with type 1 and type 2 diabetes who regularly inject insulin use insulin pens and insulin pumps. These have largely replaced the classic insulin injections.
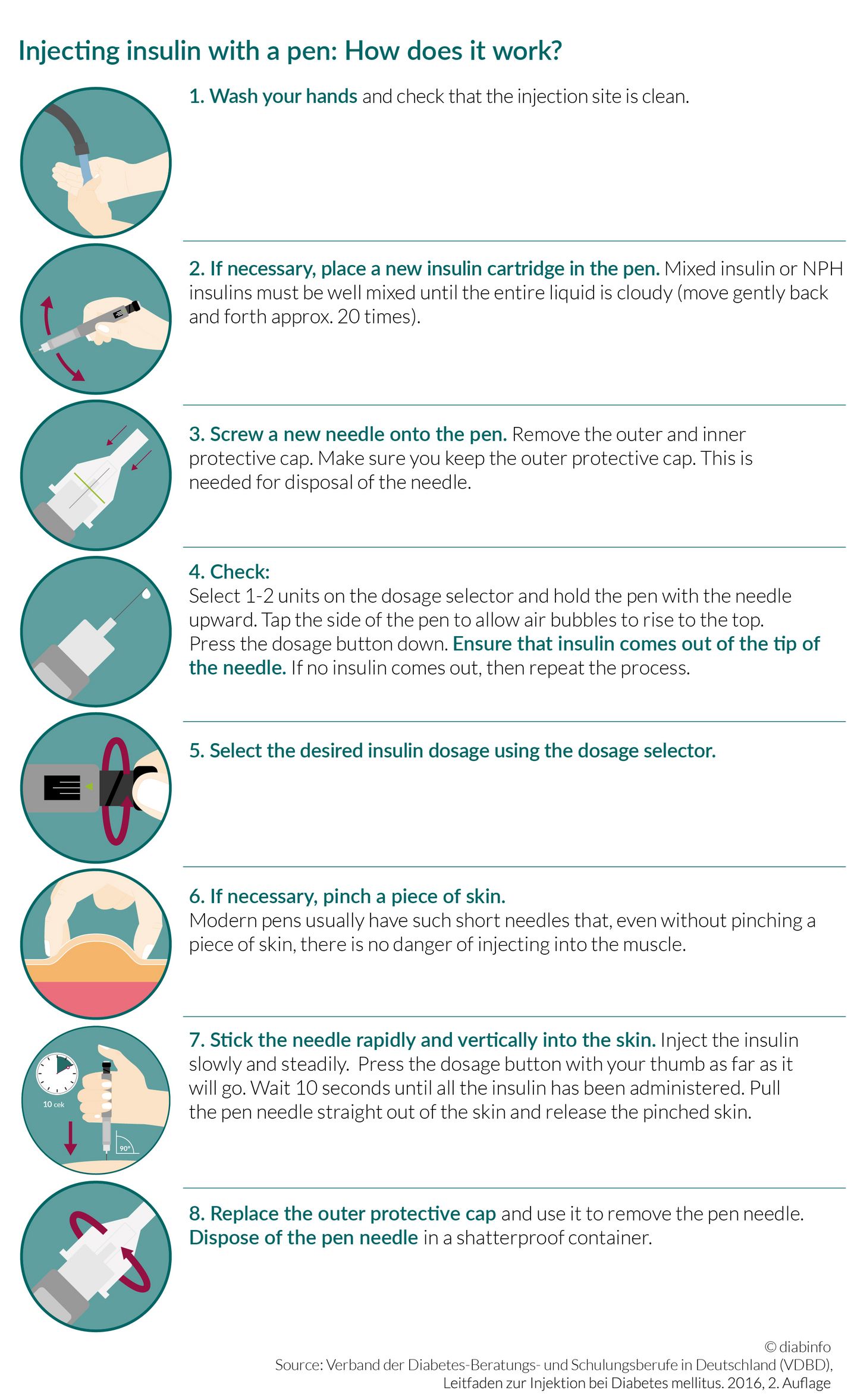
Insulin pens are easy-to-use injection aids that are about the size of a pen. The pen needles are very short and thin. The injection itself is almost painless and easy to carry out in everyday life.
Insulin pumps are small devices connected to a catheter via a tube. They replace manual injections and enable a more flexible administration of insulin.
The most modern form of insulin therapy for type 1 diabetes is the hybrid closed-loop system. This is an insulin pump connected to a continuous glucose monitor (CGM).

Injecting insulin with a pen: What models are available?
There are numerous types of insulin pens on the market. Most look similar to a ballpoint or fountain pen. Injecting insulin with an insulin pump always follows the same basic principle. However, some models do have additional functions. For example, they can store information about the amount of insulin administered. Other models can send information to a smartphone.
Semi-automatic insulin pen: The required number of insulin units can be adjusted using a dosage dial. When activated, for example, using a small lever on the side, the desired amount of insulin is injected.
Those who are fearful of injecting the small pen needle into the subcutaneous fat can use a fully automatic insulin pen. When activated, these models first inject the needle into the tissue and then administer the insulin via the cannula.
Pre-filled insulin pens also exist for which the cartridges cannot be changed. The pen is disposed of when the insulin is used up. Other types of pens can be re-filled with new insulin cartridges.
Good to know:
Your diabetes team (diabetes advisor, diabetologist, or treating physician) will be happy to advise you on which pen is best suited to you. Advice on the various available models can also be found at the pharmacy.
Insulin pumps
An insulin pump is a small device that can be attached to the waistband, for example. It is connected to a thin steel or plastic cannula via a thin tube. The cannula is usually placed under the skin of the abdomen. The pump can inject the insulin directly into the subcutaneous fat via the tube.
- An increasing number of people with type 1 diabetes, especially children and adolescents, use an insulin pump.
- The higher costs associated with insulin pump therapy must be approved by the health insurance provider in advance.
- Insulin pump therapy is often shortened to CSII (continuous subcutaneous insulin infusion).
Insulin pumps: Who are they suitable for?
Anyone who wishes to use an insulin pump must first discuss this with their treating physician. The doctor can help fill out the reimbursement application to be sent to the health insurance provider. Treatment with an insulin pump is more expensive than conventional insulin therapies using injections or pens. Health insurance companies will only assume the cost in cases of medical necessity. Insulin pump therapy is used almost exclusively for people with type 1 diabetes.
The use of an insulin pump is indicated,
- when conventional insulin therapy using the basal-bolus principle is unable to satisfactorily regulate the blood sugar levels.
- for patients with frequent blood sugar level fluctuation and episodes of low blood sugar.
- for patients with a very irregular daily routine (e.g., when working different shifts).
- for children (especially small children) who require very small amounts of insulin.
- to stabilize blood sugar levels when trying to fall pregnant or at the start of pregnancy.
- for patients with pronounced early-morning blood sugar level increases (dawn phenomenon).
- for people with type 2 diabetes who have been unable to achieve adequate diabetes management using other methods of treatment.
Insulin pumps: How do they work?
Similar to the pancreas, insulin pumps release small amounts of fast-acting insulin gradually throughout the day. This helps meet the basic insulin requirement, known as the basal rate. To meet increased insulin requirements during mealtime, a single bolus dose can be administered using the pump. The basal requirements can be preprogrammed. Bolus doses cannot be automatically administered and a button must be pressed.
- Insulin administration via the insulin pump enables the user to have a more flexible daily routine. They can adjust the amount of insulin to their needs, for example, if they spontaneously decide to exercise, or in other everyday situations, such as sleeping for longer than usual, irregular daily routines or mealtimes.
- Often, blood sugar levels can be better controlled with the help of an insulin pump than with a combination of long-acting insulin and short-acting boluses.
- Injection with a pen is no longer required when using insulin pump therapy; however, pens must still be correctly used in exceptional situations, e.g., when the pump has a technical defect.
Patch pumps: The tubeless alternative
A patch pump is a pump system that does not use tubes. The small pump is stuck directly onto the skin and a cannula is automatically inserted into the subcutaneous fat. The patch pump is controlled using a remote control. When the insulin is used up, the pump must be removed no more than 3 days later and thrown away. The benefit is that the tubes, which some find annoying, are not needed and there is no longer a risk of snagging or kinking.
Potential insulin pump risks
The use of an insulin pump can also have disadvantages. Some people don’t like having to always wear the device on their body. However, it can be disconnected for short periods, for example, when taking a shower.
The cannula injection site can become infected. This happens especially in cases where the same cannula has been used for an extended period of time or hygiene is inadequate. The cannula can also become blocked or slip out of the subcutaneous fat without the wearer noticing. If not noticed in time, this can result in high blood sugar levels or, in the worst case, diabetic ketoacidosis (hyperacidification of the blood).
Hybrid closed-loop systems
Hybrid closed-loop systems are the most modern insulin therapy for type 1 diabetes. They have an insulin pump connected to a continuous glucose monitor (CGM system). Based on the glucose level, the current insulin action, and other factors, the insulin pump administers the required amount of insulin at one-minute intervals. This enables hybrid closed-loop systems to administer the basic insulin requirement (basal rate) accurately and automatically. The therapy is supported by adjustable warning signals to warm when levels are too high or too low. Patients benefit from stable blood sugar levels and fewer episodes of high or low blood sugar.
However, hybrid closed-loop systems are not fully automatic. Before mealtimes, the user has to enter the amount of carbohydrates they will consume. The system is able to automatically counterbalance small protein-rich snacks. High target levels can be set for physical activity and exercise.
There are already several hybrid closed-loop systems available in Germany. Under certain conditions, they may be subsidized by the statutory health insurance companies.
Many diabetes patients hope that future automated pump systems will be able to completely take over the role of the pancreas. These types of devices are called artificial pancreas system, artificial pancreas and closed-loop system.
Find out more about continuous glucose measurement (CGM systems) here.
Insulin pumps: Training programs
At the start of insulin pump therapy, the users receive extensive training.
- There are structured training programs that last several days. The training courses are also suitable for people with type 2 diabetes.
- The courses can be on an outpatient or inpatient basis.
- Outpatient courses offer the advantage that patients can maintain their daily routine and adjust their basal rate better to everyday situations.
However, in hospital, accurate measurements during the night are possible. A daily routine and fewer disruptions than in everyday life at home facilitate identification of the basal rate.
What are do-it-yourself AID systems?
DIY AID stands for do-it-yourself automated insulin delivery, homemade automated insulin pumps.
The approval processes for devices that carry out sensitive functions, such as insulin administration for people with diabetes, are very lengthy. Before a product can be sold, it must go through a wide range of safety tests.
- However, there is a worldwide community of tech-savvy people (known as loopers) who, at their own initiative and independent of manufacturers, combine existing technologies to create an “artificial pancreas” and make these “homemade” closed-loop systems for their own use.
- These types of do-it-yourself system are not officially approved medical products. Their use raises a wide range of legal questions and uncertainties for both the users and their treating physicians. This is especially true when people come to harm as a result of a malfunction of the system.
The German Diabetes Association (DDG) has produced a position paper (Link in German) that deals with these legal consequences.
Sources:
Arbeitsgemeinschaft Diabetes & Technologie der Deutschen Diabetes Gesellschaft: https://www.diabetes-technologie.de (Letzter Abruf: 12.10.2022)
Bergenstal, R. M. et al.: Safety of a Hybrid Closed-Loop Insulin Delivery System in Patients With Type 1 Diabetes. In: JAMA, 2016, 316: 1407-1408
Deutsche Diabetes Gesellschaft et al.: S3-Leitlinie Diagnostik, Therapie und Verlaufskontrolle des Diabetes mellitus im Kindes- und Jugendalter. Langfassung. 2015
Heinemann, L.: Diabetes-Technologie: Stand der Dinge. In: Diabetologie, 2018, 13: 329-342
Heinemann, L. et al.: Glukosemessung und -kontrolle bei Patienten mit Typ-1- oder Typ-2-Diabetes. In: Diabetologie, 2018, 13: S97-S119
Sengbusch, S. et al.: AID-Systeme – Was können Sie heute schon, was dürfen wir erwarten? In: Kompendium Diabetes 2022, 2022: 38-44
Universitätsklinikum Tübingen, Medizinische Klinik IV: Schulungsmaterial der Diabetesambulanz
As of: 28.10.2022






